It’s time to stamp out the COVID-19 bug – not simply chase it under the fridge. Left to lurk in the shadows, this lethal infection will continue to spread, so self-isolating while waiting for a miracle vaccine is not a sound strategy. (Such a passive “herd immunity” approach will inevitably result in many avoidable deaths among the herd). Instead, a more aggressive screening approach involving testing, tracing and isolating all infected cases will minimize resulting deaths and economic consequences. Ending lockdown and minimizing mayhem will require a sound cost-effective approach for contact tracing and testing.
The key question remains: how to develop an efficient testing strategy to enable such an aggressive screening approach?
One promising solution is risk-weighted pooled testing, which uses scarce testing resources to best effect. Provinces are currently using ad hoc testing to confirm diagnosis (ie. health care and nursing homes), whereas a pooled testing approach would use a systematic two-stage method aimed at containing disease spread in the broader general population.
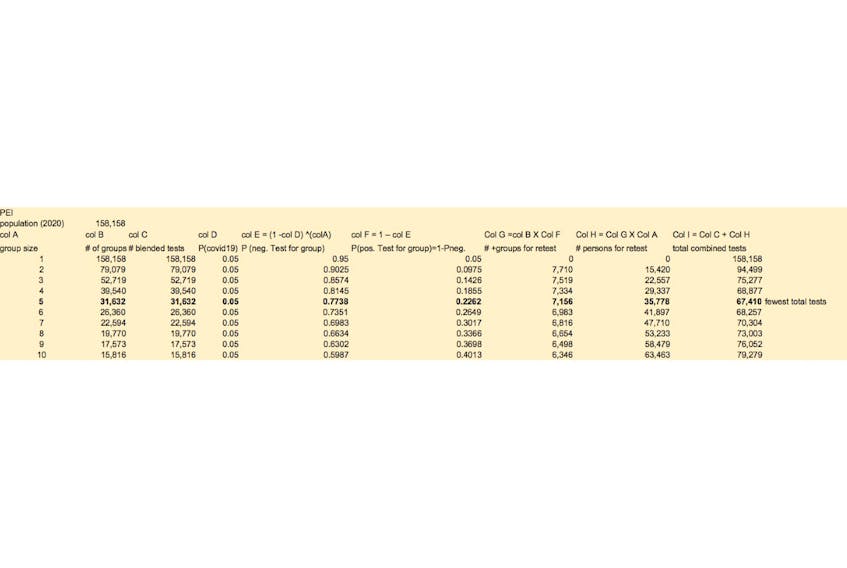
First, individual nasal swabs samples drawn from a group of individuals would be combined into one “blended” sample, and then tested as a single pooled sample. Second, for those groups with a positive “blended” result, all group members would then be retested to identify specific infected persons for 24/7 quarantine and contact tracing. Since roughly five per cent of Canada’s general population is infected (ie. true prevalence, not official reported cases), most group samples will likely be negative – requiring no further testing. Retesting can then proceed to “find the bugs under the fridge” among the other remaining positive-infected groups. This approach is illustrated in the accompanying table for P.E.I., concluding that the optimal cost-effective group size is 5 (scenario with the fewest total combined tests, assuming five per cet prevalence). As COVID-19 prevalence decreases, group size increases (ie. groups of eight for two per cent prevalence).
Rather than assuming constant five per cent average probability of infection, pooled sampling could likely be further improved upon by varying group size based on prospective COVID-19 risk. This aspect of the bug hunt draws upon my seven years experience as lead researcher developing CANRISK – a risk scoring strategy aimed at detecting prediabetes and undiagnosed diabetes in Canada.
There are strong parallels between screening for undiagnosed diabetes and COVID-19. In both cases, it is impractical to test the entire population – due to the enormous expense involved, and other practical clinical constraints. Both diseases also affect less than 10 per cent of the population, so it is more cost-effective to use a triaged, two-stage screening approach than it is to use ad hoc universal screening. Staged screening recognizes that disease risk is concentrated in certain groups, and this risk can be reliably predicted using risk factor surveys. For instance, over 80 per cent of new diabetes cases will result from just 10 per cent of the population – those with high levels of obesity, non-white ethnicity, positive family history, advanced age and other surveyed risk factors.
Pooled group testing can therefore be improved, by risk-stratifying individuals into “similar risk” groups for pooled testing. In order to developing a composite risk score (eg CANRISK), individuals applying for a COVID-19 test would first complete a risk assessment questionnaire, measuring Yes/No responses to discrete separate risk factors. (Note: all provinces currently have online “self-assessment tools” for COVID-19, but these include lumpy vague lists of grouped symptoms and are not well-suited to estimating risk scores using scientific statistical methods).
Results from subsequent tests would then be fed back for analysis, so that the relative strength of association between individual risk factors and “positive infection” could be calculated (ie relative risk). For example, “obesity” (vs normal body weight) would reflect higher risk, and so would “age” and “male gender”. Conversely, “daily smoking” would (perversely) be expected to reduce risk, based on other recent evidence. Rather than consider each of the risk factors one-by-one, a composite weighted risk score that encompasses all factors would be estimated, generating a single numeric score.
The composite COVID-19 risk score could then be used to predict positive cases within untested groups of “statistically similar” persons. Those falling into “high risk” groups (eg older, overweight, male, recent traveller, etc) would have a higher probability of positive infection -- so group size would be smaller, to reflect the increased likelihood of retesting of individuals following a positive result for the entire group (ie. blended blood sample). Conversely, group size for persons in a “low risk” group (eg. younger, normal weight, etc.) could be relatively large – reflecting the lower likelihood of a positive group result. The group size of various low/medium/high risk groups could be fine-tuned over time based on ongoing empirical feedback from actual testing. This cost-effective approach will ensure that scarce testing resources are focused on those highest risk individuals with the greatest ability-to-benefit. The pooled testing approach will also effectively triage the testing effort, so that all of the bugs under the fridge can be effectively hunted down in a systematic fashion.
One important caveat regarding the above pooled approach concerns the Health Canada approvals necessary to apply blood PCR tests for a “blended” blood sample of a group of individuals: currently, only individual testing has been approved for clinical purposes. (South Korea, Germany and Nebraska are already using pooled PCR testing). Recognizing the great health impact posed by the current pandemic, I am hopeful that any bureaucratic obstacles can be quickly swept aside (hopefully before the nasty bug escapes into the living room).
Chris Robinson is a health economist and sessional instructor at UPEI's department of economics.
EDITOR'S NOTE: This opinion piece was changed after the initial publication to reflect the fact that COVID-19 testing is done by nasal swab, not blood tests.