CHARLOTTETOWN, P.E.I. - Four new community access centres or hubs will be operational by 2020 as part of a $100-million plan to improve care for Islanders who experience mental health and addictions challenges.
Government announced the investment two weeks ago as part of its 2019-20 capital budget but revealed its many highlights during a press conference on Tuesday in Charlottetown.
The idea is to reduce the wait times in acute care hospitals and bring care closer to the homes of Islanders. The wait time for mental health care at the Queen Elizabeth Hospital is about 30 hours, slightly less in Summerside.
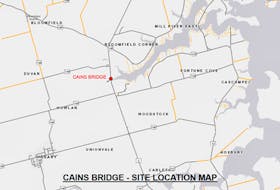
Health P.E.I. announced four community access centres/hubs will be operational sometime in 2019-20. These centres will provide robust collaborative community-based mental health and addiction services, treatments, rehabilitation and supports. They will be located in Charlottetown, Summerside, West Prince and Kings County.
“We’ll be assessing what our current infrastructure is and may look at leasing or renting depending on what we see when we do that assessment,’’ said Verna Ryan, CAO of mental health and addictions for the province. “We have a concept of 12-hour, seven-day-a-week hubs where people can have access to community mental health staff to online supports.’’
Dr. Heather Keizer, psychiatrist and Health P.E.I.’s chief of mental health and addictions, said ideally they want these hubs to be places where people can go, have access to more than one service, have a coffee and make contact with a social worker who can fill out their paperwork.
“They might be able to see their family doctor as well as their mental health worker,’’ Keizer said. “So, we reduce stigma but increase accessibility.’’
There will also be a new structured housing unit and adult day treatment program site operational in 2020-21. It will be an eight-bed structured housing facility on the grounds of the current Hillsborough Hospital providing care for patients with complex needs as they transition from hospital to the community and day treatment for patients who don’t require hospitalization.
“This may be an idea for people in crisis but don’t want to stay in hospital,’’ Keizer said. “They could go to an outpatient day program from 9-5 every day, get checked for their medications, have intense programming and get really appropriate treatment but not have to be admitted to hospital.’’
By the numbers
- 12,000 – referrals in 2016-17 to community mental health and addictions. 43 per cent were for addictions care and 57 per cent were for mental health care
- 12,000 – people who presented with mental health and addiction issues in 2016-17. Only half were seen
- 600 – An approximate number of Islanders who visited a mental health walk-in clinic in 2017
- 300 – Seniors who have been referred to the Seniors Mental Health Resource Team since April 2016
- 900 – The approximate number of clients served in the four opiate replacement program clinics in Montague, Mount Herbert, Summerside and Charlottetown
- 4,000 – Students who have received help from the Student Well-Being Teams last school year (October 2017-June 2018)
- 1,014 – The number of Island youth and families the Strongest Families Program has supported since October 2015
- 29 – clients who have completed the first 16-week cycle of the Insight Program, P.E.I.’s Youth Mental Health Day Treatment Program, with each receiving intensive therapy five days a week. It opened in Charlottetown in October 2016
There will be a new dedicated mental health and addictions emergency department and acute stabilization unit that will be operational in 2021-22. It will be a 12-bed dedicated department (eight emergency treatment spaces and a four-bed stabilization unit) to be co-located at the Queen Elizabeth Hospital in Charlottetown. It will provide dedicated and timely access to trained mental health and addictions clinicians.
Mobile crisis units will also be put in place. Health P.E.I. is working on a model now involving stakeholders from police, 911, Island EMS and other partners. The teams should be in place sometime next year. Keizer said these teams could reduce visits to the emergency room by 60 per cent.
Long-term housing with community mental health supports for people living with mental illness is also part of the plan and should be in place by 2021-22 and 2022-23.
“If we were able to provide them with housing in the community they’d have a better quality of life,’’ Keizer said.
Ryan said beginning next year they’ll look at expanding some of their transitional housing and possibly infrastructure on the grounds of the Hillsborough Hospital.
In addition, a new provincial acute mental health and addictions hospital will be constructed to replace the aging Hillsborough Hospital. It’s slated for completion by 2024-25.
Already available is e-mental health solutions such as rural tele-mental health services, online self-scheduling, virtual therapies and peer counselling.
Government is investing about $450,000 this fiscal year to carry out infrastructure planning for new program sites and facilities in regard to the entire five-year plan. The more detailed infrastructure plan will include specific locations, proposed designs and budgets for each component. New infrastructure will be phased in over the next five years appreciating that some components, such as the mental health and addictions emergency department and hospital, will take longer to build.
Related: Disability Support Program gets new name, larger scope