SYDNEY, N.S. — In the fall of 1918, people waited anxiously across Canada for their loved ones to return from the First World War.
Unfortunately, some of those happy reunions had deadly consequences.
As if the First World War wasn’t bad enough, the aftermath for much of the world ended up being worse, thanks to one of the deadliest influenza epidemics the world has ever experienced — the Spanish influenza. Highly contagious, it spread easily from the soldiers who picked it up while fighting in Europe and gave it to their loved ones who joyfully greeted them when they arrived home from the war.
Consider this: The First World War killed about 40 million people over a four-year period. Spanish flu is thought to have killed between 50 and 100 million people over a three-year period, 1918 to 1920, at a time when the world’s entire population was 1.9 billion.
“The soldiers who came back from the war, came by ship into Halifax and immediately boarded a train and travelled across Canada,” says Halifax-based medical history researcher Dr. Allan Marble, who is working on a book that includes a chapter on the Spanish influenza.
“When they got into Manitoba, Saskatchewan and Alberta, British Columbia, their relatives would know they were coming and they would be down at the train station waiting for them and when they got off the train, everyone was hugging them and kissing them and the health officers were frustrated. ‘We can’t do anything about this — they’re just spreading the virus, and we can’t control the crowds.’ So as a result, it spread like wildfire in Saskatchewan and Alberta. Ontario, Nova Scotia and New Brunswick had the lowest death rates and I think they learned a lot from Nova Scotia’s experience because it hit Nova Scotia first in Canada.”
And the first one to die in Nova Scotia was a Cape Bretoner.
FIRST ONE TO DIE

It happened in a tiny community far away from the ravages of war. Margery MacDonald of Belle Cote was only 26 years old when she died from the Spanish influenza on Sept. 1, 1918.
Not much is known about her but it is believed she contracted it from a soldier, perhaps a friend or a relative, returning home from the war.
“This was the way the disease spread of course — in Nova Scotia it was the returning soldiers from the First World War so this soldier by the name of Murdo MacDonald, he apparently was from Inverness County and he had been injured and he was sent back to Cape Breton and he arrives at Belle Cote or the general vicinity probably a week before and he’s carrying the virus. And of course, he doesn’t know it and he brings it into the community and of course, the community members have no immunity at all to the Spanish influenza so within two weeks, there were either 12 or nine deaths from Spanish influenza in Inverness County near Belle Cote. That’s the first outbreak of Spanish influenza in the province.”
There would be more.
MORE DEATHS

In addition to soldiers coming home, the flu arrived on Nova Scotian shores in the fall, a busy time in the fishery.
“At that time, the Gloucester fishermen from Massachusetts were constantly arriving at all the fishing ports around Nova Scotia and they would drop in while they were fishing to buy their supplies,” said Marble. “Since the Spanish influenza had broken out in Massachusetts about a month before it broke out in Nova Scotia they were again bringing the virus into Nova Scotia. Yarmouth was one of the first to start realizing that it’s here and it’s now in western Nova Scotia. Because once one person came down with it those people who were trying to care for that individual took the virus home with them, not knowing. The next place that really suffered from it was Petit De Grat Island because the Gloucester fishermen were coming in there too.”
During the month of October, more than 30 people died in Petit de Grat Island.
IN THE NEWS

Even in the days long before cell phones, the internet and television, news of the deadly new illness spread quickly.
Sydney Daily Post, 29 October 1918: “Nine Funerals In One Day at Little Village of Petit de Grat” — Seven deaths on Sunday and two on Monday from Spanish influenza in Petit de Grat … The poor victims had not even the comfort of religious consolation …
Apparently, four of the victims came from the same home. A few days later, the Halifax Evening Mail mentions that in Petit de Grat, which was home to about 100 families, 25 people had died and more were seriously ill.
“Whole families are stricken with the disease.”
And let’s not forget about Dr. MacKenzie, a health officer from Pictou, who was trying to find ways to alleviate the dreaded outbreak in his area.
“He had held a meeting on a Thursday night of his health board and they were trying to decide how they were going to deal with this outbreak so that’s Thursday night,” says Marble. “The next day, he didn’t come to his office to go to work and when they went to his house, they found him dead in bed from the influenza. So he probably had the influenza during the meeting and it killed him during the night.
“And he was a man 35 years old - he was a young healthy man.”
NOT JUST A FLU

As reports of COVID-19 saturate the airwaves and toilet paper and hand sanitizer disappear from store shelves, there may be a temptation to say, ‘get a grip — it’s only a flu.’ And while Spanish flu may have killed more people than the Halifax Explosion, we all know something like that could never happen again, right? After all, we’re so much more advanced medically and things are so much better today.
Yet, when Spanish flu arrived in Louisbourg back in 1918, people could go to the Louisbourg Marine Hospital for treatment. It was a facility that was surprisingly advanced for its time, says Chris Bellmore, president of the Sydney and Louisbourg Railway Historical Society.
“It did see some patients with the Spanish flu,” says Bellemore. “I don’t have a real record of how many but there was a quarantine officer during that whole period that was in Louisbourg at that time, Dr. D.A. Morrison. They had a quarantine officer here as part of the operations of the hospital which is important to note.”
The fact a small community like Louisbourg had its own hospital and a quarantine officer on staff is a testament to the times — there were still occasional outbreaks of smallpox and other contagious diseases to deal with and throughout Nova Scotia, efforts had been made to remain prepared.
“They had a very rigorous health standard — they had some forethought when it came to health legislation and that really helped them out,” says Bellemore. “They had a lot of policies in place around quarantine and stuff — they were ahead of their time in comparison to places like Ontario where people suffer a lot more and it was because they didn’t have a lot of legislation and policies around these types of things. That’s an important point to make too. Nova Scotia was really seen as a national leader in those areas at that time.”

Nova Scotia had the lowest mortality rates of any place in North America from the Spanish flu, something that Marble attributes to doctors being in positions of influence at that time.
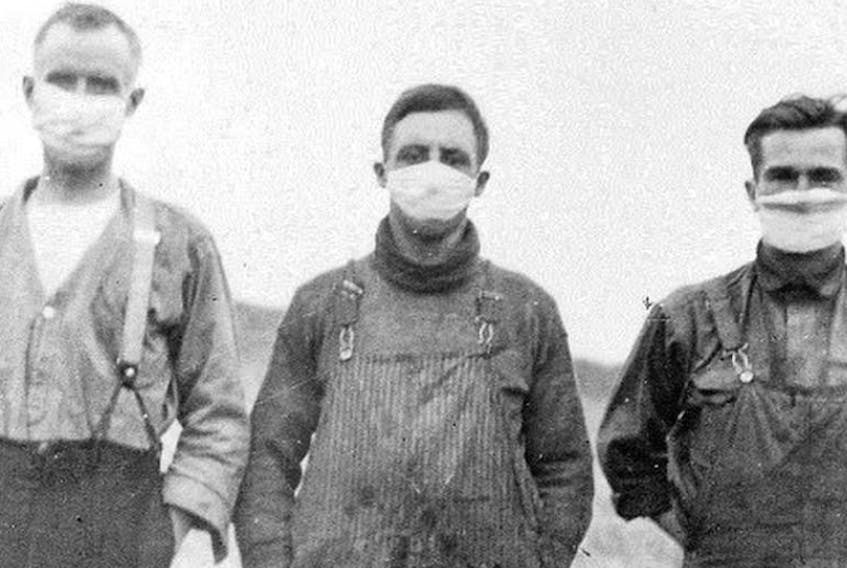
“They decided right away that this was a major crisis and they were going to do something to try to prevent people from coming down with this flu,” said Marble. “They found out what was going on in Boston and they said immediately that we’re going to close all the schools, churches, universities, bowling allies, just everything and they did that for six weeks. And once they did that in Halifax the mayors of all the major towns in Nova Scotia did the same thing including Sydney and Glace Bay and so everything was closed for six weeks and in their newspaper articles they pointed out that the most important thing to do was to isolate yourself and your children. Don’t communicate with anyone or physically come near anyone, just completely stay inside your house and don’t even read your mail or accept your mail from the mailman because he may be carrying the virus.”
As a result, 2,230 Nova Scotians died over the three year flu period (1918-1920), for an overall death rate of 3.16 per thousand, considerably lower than the death rate in the U.S. which was 6.2 per cent per thousand. Some parts of Nova Scotia like Richmond County had a death rate of 5.3 per thousand and Cape Breton, in general, came in at 4.2 per thousand. Parts of western Canada had rates over 6 or 7 per thousand. If it hadn’t been for this province’s efforts to prevent crowds and keep the population isolated and less likely to infect others, the rates might have been a lot different.
“In our generation, we really haven’t been exposed to these things but it was a way of life for people back then,” Bellemore says.
“They had a better understanding of what these things were and people in many cases knew what they had to do to protect themselves. I think over the last 100 years we’ve been very privileged to not be a part of that world but with that, we’re less prepared.”
HIGH MUTATION RATE
While it may be some time before a vaccine or cure for COVID-19 is available, avoiding people, washing hands, not touching your face and maintaining sanitary surroundings seem to be just as valid today as they were in the past and maybe the best way to keep it at bay.

According to Dr. Chris Lata, an infectious disease specialist based in Sydney, there are considerable differences between the Spanish flu and COVID-19 but there are a few similarities. Both are viruses and both are contagious.
“The coronavirus is actually from a different family of viruses than the influenza viruses are from,” says Lata. “The influenza virus was the virus responsible for the Spanish flu and for the pandemic strain of influenza that took out a great degree of the world’s population in 1918 so they’re different families and the genetic makeup and the way the virus particle looks is different as well. The influenza virus is a little bit more hardy and lives more easily on surfaces which makes it easier to spread. And it is spread by droplets or people’s coughs and secretions.”
But to say COVID-19 is just another type of flu isn’t accurate either.
“The reason influenza can survive longer is that it is a non-enveloped virus — it is an RNA virus much like the coronavirus is but it is a different type of RNA — the coronavirus is an enveloped virus and it is also an RNA virus but it is a different type of RNA or a different configuration and so its lifespan and infectious parameters are slightly different than influenza. In terms of the genetic family that they’re from, they’re completely different viral particles, they’re from different families.”
RNA viruses can easily mutate by accidentally changing their protein structures or by changing some of the viral coat that can attach and infiltrate human cells. It’s that ease of mutation that leads to new flu strains all the time and which has led to previous coronaviruses like the SARS virus.
“That mutation and cross-mixing of the RNA structure which is like the DNA of the virus can mix in different hosts very easily and so that’s what makes the mutation rate of influenza particularly high, much, much higher than other viruses and that is why it is so difficult to keep up with the vaccinations,” says Lata. “(It’s) why we need a new shot every year — the strain changes so quickly with the mutations in different reservoir hosts that it changes that protein structure very fast.”
But while a new flu strain every year can be simply annoying because of the continuing need for an annual flu shot, there remains the chance that one of those strains will emerge as one that is much more dangerous.
“The likelihood that a very relevant pathogen that causes a pandemic type of outcome with influenza is actually very high,” says Lata. “That’s actually one of the reasons that the WHO and CDC and pretty much virologists around the world fear influenza more than any other pathogen in the world because that is the most likely pathogen to create an event like the Spanish flu that takes out a large degree of the population.
“And the reasons for that are twofold: one, the mutation rates are high and the likelihood of coming up with a strain that does those things is optimal and the other thing is that the world is different than it was at the time of the Spanish flu.”
MANY DIE BUT MORE RECOVERED

The Spanish flu of 1918-20 infected between one-fifth and one-third of the world’s population during a time when the world’s total population was 1.9 billion. While the full impact of COVID-19 won’t be known for some time, it must be remembered that we now live in a much more mobile society that would allow it to spread more completely and more quickly. Yet, thanks to better knowledge and health care, we can also counter and deal with it much more quickly.
Age is one of the major differences between the two illnesses. COVID-19 seems to adversely affect those who are elderly and already suffering from illnesses while Spanish flu aimed for those between the ages of 15 and 40 — supposedly society’s healthiest people.
“That sounds strange but it took quite a few years before a medical doctor in Australia came up with a theory that I agree with,” says Marble. “It’s called massive immune response. What that means is that when you’re a young person between 15 and 40 and usually considered the healthiest people, when they were attacked by the influenza virus, their body reacted vehemently, so fast to build up antibodies against the antigens of the virus that they actually drowned in their own blood. They hyperventilated so much that they were actually causing blood to go from their pulmonary arterial and venous systems right through the lining of their lungs into their lungs and so their lungs filled with blood. And of course, they drowned in their own blood. They couldn’t breathe.”
Ironically, those over 40 fared much better.
“They were alive during the Russian influenza of 1890 and as a result, they had built up antibodies against it,” says Marble, adding Russian influenza was similar to Spanish influenza in the type of flu that it was. “They already had immunity to the Spanish influenza so they could fend it off whereas the people under 40 couldn’t.”
The mortality rate for Spanish flu has been estimated to be between 2.7 and 5.4 per cent. Although deadly for some, many did recover. On Sept. 30, 1918, 1,200 had developed it in the town of Inverness and 10 subsequently died.
And while many associate Spanish flu with 1918, it actually lasted in Nova Scotia until around May 1920 when it finally disappeared.