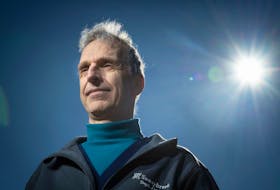
Cheap, rapid COVID-19 tests simple enough to use anywhere — home, school, the office — could help us climb out of the pandemic disaster, says infectious diseases specialist Dr. Andrew Morris. Just spit into a tube or swab your nose, wait a few minutes for the stripes to change colour — results available within minutes.
With no vaccines or “fantastic therapies” for COVID, the best we can do is keep infected people out of buildings to prevent them from unknowingly spreading the virus, says Morris.
Which is why he finds it “absurd” that Heath Canada says the risks of home or self-testing kits outweigh the benefits and that it will reject applications for such devices “without compelling new evidence to the contrary.”
The federal health agency worries that, “without the guidance of a health-care professional,” people would use the home test kit improperly or “misinterpret the results” and that it could be impossible to collect test results — information that’s key to “important health decisions involving disease control during an outbreak,” the department said in an emailed statement.
“If it’s done in a haphazard way … you might actually create more problems, confusion than the actual benefits because you might get maybe a higher risk of false negative results,” Dr. Howard Njoo, Canada’s deputy chief public health officer, said Tuesday during a COVID-19 briefing.
Morris wants the government to seriously rethink its position on home testing. They’re not the solution to COVID, but they are part of it, he believes.
Cheap, rapid testing is the backbone of infectious disease management, says Morris, of the Sinai Health System and University Health Network in Toronto. “But if Health Canada says ‘we aren’t even interested in these tests,’ they are neither being open-minded nor strategic in understanding the potential of these tests.”
It has echoes of earlier federal dismissals of face masks, when officials worried masks would lead to a “false sense of security” and more face-touching.
“The current strategy is not to trust the public… and we need to change that,” Morris says.
The gold standard of testing today is a workhorse called reverse transcriptase polymerase chain reaction, or RT-PCR, which amplifies SARS-CoV-2 from nasal swabs, so that minute amounts of RNA can be detected. Anyone who is sick or showing symptoms of COVID-19, or who thinks he or she may have been exposed, can get PCR testing.
But PCR testing isn’t designed around getting our lives back to normal, Morris says. It’s expensive, testing capacity is seriously limited and it can take days to get results. Vancouver has seen traffic gridlock at testing sites as B.C. battles with a surge in cases. Ottawa has had four-hour-long waits at its COVID testing sites.
“The only way we can get our society back up and running is by having some better situational awareness than what we have,” Morris says.
The FDA recently granted emergency use approval to a saliva-based test developed by researchers at the Yale School of Public Health. It’s being used to test players and staff from the National Basketball Association. But it’s not a rapid test. It still needs to be processed by labs and machines.
Things will change dramatically with lateral flow assay devices, Morris says. These are inexpensive tests that work like pregnancy tests. Some are paper-based tests designed to detect viral proteins, others are designed to detect, like PCR tests, viral RNA, the genetic blueprint of the virus.
It’s meant to be a no-brainer: Yes, no. It’s a binary result
Rapid tests aren’t perfect. They aren’t as sensitive as PCR tests. But they don’t need to be perfect, argues Harvard Medical School epidemiologist Michael Mina.
Mina says the tests can detect the virus when a person is most infectious, with high viral loads. “The vast majority of PCR positive tests we currently collect in this country are actually finding people long after they have ceased to be infectious,” Mina told Harvard Magazine. Paper-strip test could cost less than one or two U.S. dollars to produce, he says. Millions could take them daily or every other day. Frequent testing, with fast results, would help break chains of transmission, Mina tweeted this week.
Morris has heard talk the FDA is expected to authorize several lateral flow assay tests for COVID-19 in the coming weeks. “And nothing by Health Canada. To me, this is a massive, massive blind spot.”
One key strategy in the COVID battle is getting people to self-assess, to check for symptoms before leaving home. “You don’t need perfect tests to improve what’s going on — you need tests that are going to be substantially better than the performance art otherwise known as temperature checks and asking people every single day the same questions about symptoms, knowing very well that there are going to be people who are largely not going to be forthright in answering those questions honestly.”
It’s also hard to imagine how people might “misinterpret” the results, he says. “It’s meant to be a no-brainer: Yes, no. It’s a binary result.”
People who test positive would be encouraged to see their doctor for additional testing and public health reporting. And while there are important concerns about false negatives, “just think about the massive number of people out there who are reassured by being asymptomatic,” Morris says.
The more true positive cases we can catch will make everywhere safer, he says.
Vancouver-based XPhyto Therapeutics Corp. has partnered with a German company to develop a rapid screening test to detect viral RNA from saliva. “We’ve been able to lower the detection threshold to a point where it essentially will catch almost all infected patients,” said XPhyto CEO and director Hugh Rogers. Results are available in less than five minutes. The U.S. Food and Drug Administration, which has called at-home COVID-19 tests a potential “game changer” requires the tests to detect at least 90 per cent of cases.
Halifax-based Sona Nanotech’s rapid COVID-19 test targets the spike protein on the surface of the virus. The Scientist reported that, in lab experiments, the test correctly identified 29 of 30 swab samples taken from healthy people as negative. When the SARS-CoV-2 virus was artificially added to the 29 samples, the test identified 28 as positive.
Canada, through its funding agencies, has been paying for research for at-home tests, including at university labs, but “the high entry barrier is discouraging innovation on at home tests — we won’t have them if & when needed,” tweeted David Juncker, professor and chair of biomedical engineering at McGill University.
• Email: [email protected] | Twitter: sharon_kirkey
Copyright Postmedia Network Inc., 2020