Top stories in Prince Edward Island
P.E.I. PCs vote down right to repair bill
A private member’s bill, which would have set out some rights for farmers to have access to the tools needed to repair machinery, has been defeated in the P.E.I. legislature.
The bill, introduced by Liberal MLA Robert Henderson, would have required ...
Updated 13 hours ago
|5 min read
Local
MoreP.E.I. PCs vote down right to repair bill
A private member’s bill, which would have set out some rights for farmers to have access to the tools needed to repair machinery, has been defeated in the P.E.I. legislature.
The bill, introduced by Liberal MLA Robert Henderson, would have required ...
Updated 13 hours ago
|5 min read
Opinion
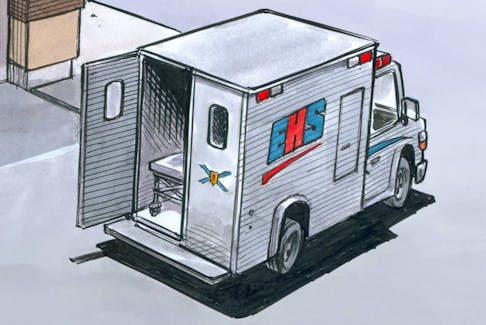
MoreBRUCE MacKINNON: Walk it back stat
Bruce MacKinnon's cartoon for April 20, 2024.
Updated 13 hours ago
|1 min read